Current Research
Structure and Function of the Distal Outflow Tract
Project Narrative
Although primary open angle glaucoma (POAG) is a leading cause of irreversible blindness from elevated fluid pressure within the eye, half the resistance to drainage of this fluid remains unexplained. Prior research focused on improving the function of a strainer tissue at the intake of the eye’s drainage system, but even complete removal through surgery fails to reduce resistance to drainage sufficiently. The proposed translational research aims to enable reduction of such resistance and expand and regenerate the drainage vessels of the outflow system, using new tools developed by the PI and delivering molecules recently discovered to play an essential role in the developing outflow system.
Project Summary
Glaucoma is a leading cause of blindness with rising prevalence, that exacts costs of $2.5 B in the US alone each year. Up to 3% of the population over the age of 50 have glaucoma and 13% by the age of 80, depending on ethnicity. There is an unmet need for better therapies because the cause of the destructive elevated intraocular pressure (IOP) in glaucoma is only partially understood. The trabecular meshwork (TM) that guards the intake of the eye's drainage system intake has long been considered the principal cause of decreased outflow in primary open angle glaucoma. However, our TM ablation studies in over a thousand patients strongly suggest that at least 50% of outflow resistance resides further downstream, distal to both TM and Schlemm’s canal (SC). The overarching goals are to identify the mechanisms of post-trabecular meshwork outflow resistance in glaucoma and to develop new therapeutic strategies for improving outflow. The distal outflow resistance has to reside either in the collector channels (CC), the intrascleral plexus (ISP) or aqueous veins (AV), collectively known as the distal outflow tract (OT). Micro-computed tomography analysis of collector channels in glaucomatous eyes revealed fewer functional outflow vessels than in healthy eyes. Insights into their origin and function point toward an as-yet unexploited similarity to blood and lymphatic vessels. Strikingly, key mediators of vasculogenesis and vasodilation are now implicated in having a role in outflow, yet none have been explored therapeutically.
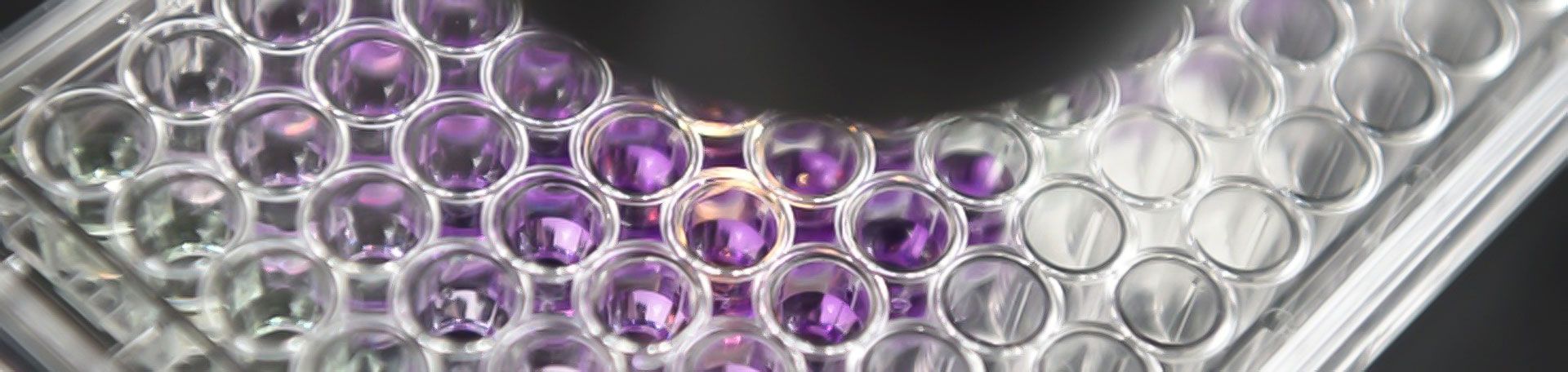
We generated new tools to accomplish this goal, including a translationally relevant porcine anterior segment perfusion system, a method to quantify site-specific outflow, a full-thickness, 3D confocal microscopy of the OT, and measurement of aqueous vasodilation. Using these, we discovered that OT dilation increases the outflow facility, even after TM ablation. Here, we aim to define factors of post-TM outflow regulation to enable new treatment strategies.
Aim 1: determine the effects of vasodilators ("X") and ("Y") on OT structures and flow regulation.
Aim 2: determine if angiogenic development can be induced by ("X") and ("Y") delivered as transgenes to generate new OT elements.
Aim 3: assess whether ("Z") can initiate OT expansion by stimulating a subclass of angiogenesis. The results will yield the first analysis of the relationship between the distal OT structures and outflow function. They will provide insight into how angiogenic and dilation pathways are regulated through transcriptome analysis. This research will enable new tools to manipulate OT structure and function in porcine and human eyes, which will improve outflow, lower IOP, and improve clinical management and outcomes in glaucoma patients.
Our Contributions to Science
Development of a Minimal Feline Immunodeficiency Viral Vector System and Scaled-up Production
Glaucoma, a leading cause of irreversible blindness, is a lifelong, progressive optic neuropathy that is caused by increased intraocular pressure. No long-term treatment was available to match its chronicity while being specific to the diseased tissues. As a postdoctoral scientist, I established high-level gene transfer with our minimal FIV vector system to the strainer tissue of the outflow tract, the trabecular meshwork. I created minimal transfer vectors for a novel lentiviral vector system based on the feline immunodeficiency virus (FIV) and explored them in eye models. I reduced the 1353 nucleotide gag gene stepwise to only 311 nucleotides needed to preserve packaging. This diminished chances of recombination with the packaging plasmid that other team members minimized. I lead and took part in several in vivo projects that showed sustained transgene function and enabled the first pressure lowering gene therapy.
- Loewen N, Fautsch MP, Peretz M, Bahler CK, Cameron JD, Johnson DH, Poeschla EM. Genetic modification of human trabecular meshwork with lentiviral vectors. Hum Gene Ther. 2001 Nov 20;12(17):2109–2119. PMID: 11747600
- Loewen N, Bahler C, Teo W-L, Whitwam T, Peretz M, Xu R, Fautsch MP, Johnson DH, Poeschla EM. Preservation of aqueous outflow facility after second-generation FIV vector-mediated expression of marker genes in anterior segments of human eyes. Invest Ophthalmol Vis Sci. 2002 Dec;43(12):3686–3690. PMID: 12454037
- Loewen N, Fautsch MP, Teo W-L, Bahler CK, Johnson DH, Poeschla EM. Long-term, targeted genetic modification of the aqueous humor outflow tract coupled with noninvasive imaging of gene expression in vivo. Invest Ophthalmol Vis Sci. 2004 Sep;45(9):3091–3098. PMID: 15326125
- Loewen, R. T., Roy, P., Park, D. B., Jensen, A., Scott, G., Cohen-Karni, D., Fautsch, M.P., Schuman, J.S., Loewen, N. A. A Porcine Anterior Segment Perfusion and Transduction Model With Direct Visualization of the Trabecular Meshwork. Invest Ophthalmol Vis Sci. 2016 Mar;57(3), 1338–1344.
Outflow Engineering for Glaucoma
The trabecular meshwork, a strainer-like tissue at the intake of the outflow system, is a principal cause of increased intraocular pressure in glaucoma. My laboratory developed a conditional cytotoxic vector that ablates this structure resulting in a pressure drop. A repopulation activity and increase in cell density follow this ablation suggesting a reservoir of progenitor cells. The findings contribute to the growing evidence that ocular stem cell niches exist adjacent to or within the diseased structures. Cytoablation has allowed us to replace the trabecular meshwork by seeding it with transplanted cells. We created the first ex vivo model for a highly challenging microincisional glaucoma surgery, ab interno trabeculectomy, and developed quantitative canalograms to measure the enhancement with a high spatial resolution. We used this technique to establish outflow tract vessel transduction and progenitor seeding. We correlated our functional studies to morphometric analyses of whole specimen ribbon-scanning confocal microscopy. These massive datasets indicated that proximal outflow structures had greater diameters nasally while the venous plexus was larger in the inferior limbus.
- Zhang Z, Dhaliwal AS, Tseng H, Kim JD, Schuman JS, Weinreb RN, Loewen NA. Outflow tract ablation using a conditionally cytotoxic feline immunodeficiency viral vector. Invest Ophthalmol Vis Sci. 2014 Feb;55(2):935–940. PMCID: PMC3929079
- Loewen RT, Brown EN, Scott G, Parikh H, Schuman JS, Loewen NA. Quantification of Focal Outflow Enhancement using Differential Canalograms. Invest Ophthalmol Vis Sci. 2016 May 1;57(6):2831-8. doi: 10.1167/iovs.16-19541. PMID: 27227352
- Waxman S, Loewen RT, Dang Y, Watkins SC, Watson AM, Loewen NA. High-Resolution, Three Dimensional Reconstruction of the Outflow Tract Demonstrates Segmental Differences in Cleared Eyes. Invest Ophthalmol Vis Sci. 2018 May 1;59(6):2371-2380. doi: 10.1167/iovs.17-23075. PMID: 29847643
- Waxman S, Wang C, Dang Y, Hong Y, Esfandiari H, Shah P, Lathrop KL, Loewen RT, Loewen NA. Structure-Function Changes of the Porcine Distal Outflow Tract in Response to Nitric Oxide. Invest Ophthalmol Vis Sci. 2018 Oct 1;59(12):4886–4895. PMCID: PMC6181305
Techniques and Outcomes of Microincisional Glaucoma Surgery
Progress in microengineering has allowed manufacturing surgical devices small enough to ablate the trabecular meshwork, the primary outflow resistance in glaucoma. However, despite removal over up to 180 degrees early and late failures are common even in experienced hands. Evidence points towards an overlooked resistance from outflow tract elements that are downstream of the trabecular meshwork and can regulate flow. We identified risk factors and expanded indications for ab interno trabeculectomy that have led to broader usage even in glaucomas with a relative contraindication, for instance, glaucomas with narrow angles. I was the principal investigator for these research projects that analyzed outcomes in more than 1000 patients.
- Parikh HA, Bussel II, Schuman JS, Brown EN, Loewen NA. Coarsened Exact Matching of Phaco-Trabectome to Trabectome in Phakic Patients: Lack of Additional Pressure Reduction from Phacoemulsification. PLoS One. 2016 Feb 19;11(2):e0149384. PMCID: PMC4760733
- Loewen RT, Roy P, Parikh HA, Dang Y, Schuman JS, Loewen NA. Impact of a Glaucoma Severity Index on Results of Trabectome Surgery: Larger Pressure Reduction in More Severe Glaucoma. PLoS One. 2016 Mar 23;11(3):e0151926. PMCID: PMC4805208
- Neiweem AE, Bussel II, Schuman JS, Brown EN, Loewen NA. Glaucoma Surgery Calculator: Limited Additive Effect of Phacoemulsification on Intraocular Pressure in Ab Interno Trabeculectomy. PLoS One. Public Library of Science; 2016 Apr 14;11(4):e0153585. PMCID: PMC4831696
- Esfandiari, H., Shazly, T., Waxman, S., Kola, S., Kaplowitz, K. B., Brown, E. N., & Loewen, N. A. (2018). Similar Performance of Trabectome and Ahmed Glaucoma Devices in a Propensity Score Matched Comparison. J Glaucoma. 2018 Jun;27(6):490-495. doi: 10.1097/IJG.0000000000000960. PMID: 29613976
Operator:
+49 931 201-20351
How to get an appointment?
Outpatient and inpatient appointments:
Private patients please call
+49 931 201-20602
For Children's Appointments and all questions regarding Strabismus and Neuroophthalmology please call
+49 931 201-20487
Address
Department of Ophthalmology | University Hospital Wuerzburg | Josef-Schneider-Str. 11 | Building B2 | 97080 Wuerzburg | Germany